Total Hip Replacement
Today total hip replacement is recognised as one of the most successful surgical procedures. The success story of total hip replacement started in the 1960s and since then there have been significant developments in numerous aspects of the total hip replacement procedure and peri-operative care. In the United Kingdom on average 100,000 primary hip replacements are performed each year with the current generation of prostheses expected to last at least 20 years in more than 90% of patients.
When should I consider having hip replacement?
Your GP, first contact practitioner, physiotherapist, osteopath, or surgeon will diagnose arthritis in the hip and suggest hip replacement as an option if non-operative treatment measures have failed. The surgeon will discuss the pros and cons of continuing non-operative treatment and of undertaking operative treatment i.e. total hip replacement. The decision to have a total hip replacement for hip arthritis is entirely yours and you may wish to seek the advice or opinion of your family to help you decide.
Total hip replacement for hip osteoarthritis is considered if:
- There is persistent pain due to hip osteoarthritis at rest. Pain might also affect sleep
- Pain restricts physical activities like walking and even low impact exercise
- Stiffness in the hip restricts day to day tasks like wearing shoes etc.,
- Quality of life is considerably adversely affected due to the above symptoms
- Non-operative treatment measures have not helped
- A patient is unable to tolerate non-operative treatment e.g. reaction to pain killers
Total hip replacement is also undertaken to treat specific types of broken hip (fracture of neck of femur) in certain groups of patients. This is performed as an urgent procedure unlike that done for hip osteoarthritis.
Can I delay the hip replacement?
Hip osteoarthritis is not a life-threatening condition. It is, however, a disabling condition which almost always becomes progressively worse over time and limits your activities. Hip replacement is undertaken to improve the quality of your life and so it is entirely your choice whether and when to have total hip replacement. Only occasionally, in conditions such as rapidly progressive type osteoarthritis or osteoarthritis with secondary avascular necrosis, might the surgeon advise you to have the hip replacement earlier rather than later. This is to avoid gross damage to the hip which could make hip replacement more complicated.
Although it is advisable to delay hip replacement as much as one can without compromising quality of life too much, age is not a limiting factor. The average age of patients undergoing hip replacement is around 68 years with 60% of patients being female. Mr Velayudham’s patients’ age range from those in their teens to patients in their ninety’s.
What does the actual procedure involve?
Digital templating is carried out to plan the exact placement of correctly sized prostheses for the patient to achieve stable fixation, placement at correct angles in all three planes, correct leg length and soft tissue tension. Robotic or computer-assisted surgery helps the surgeon to execute the procedure more accurately. This is still evolving, and Mr Velayudham uses computer-assisted surgery where appropriate.
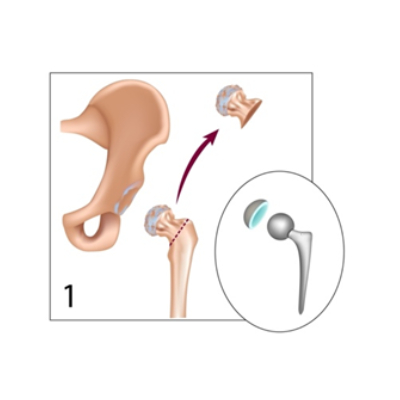
The procedure involves replacing the cartilage and part of the bone forming the joint with artificial parts. Under anaesthesia the joint is exposed through an approach that is safest, does not affect the hip function and has less chance of complications. The ball (head of the femur) of the hip joint is removed (Fig 1).
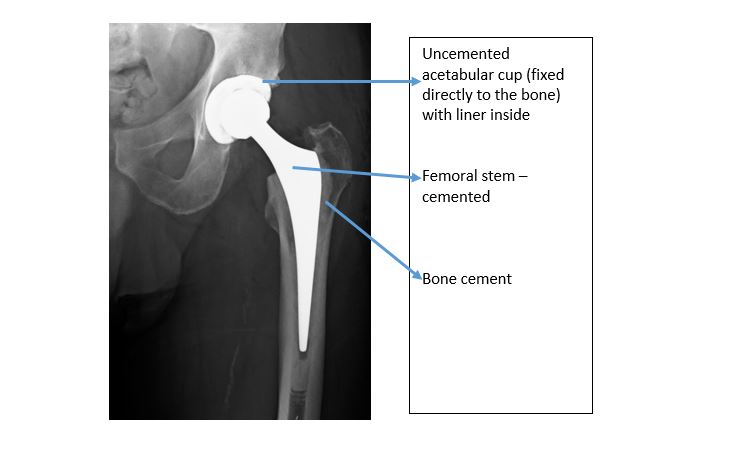
The socket (acetabulum) is cleared of residual cartilage and prepared to seat the artificial socket. The correct size of socket for the patient is seated in. Fixation to the bone can be a cemented or uncemented type of fixation. The femur canal is prepared. The femoral stem component is inserted into the canal (Fig 2 and 3). The artificial ball (femoral head component) is coupled to the top end of the metal stem after trial reduction.
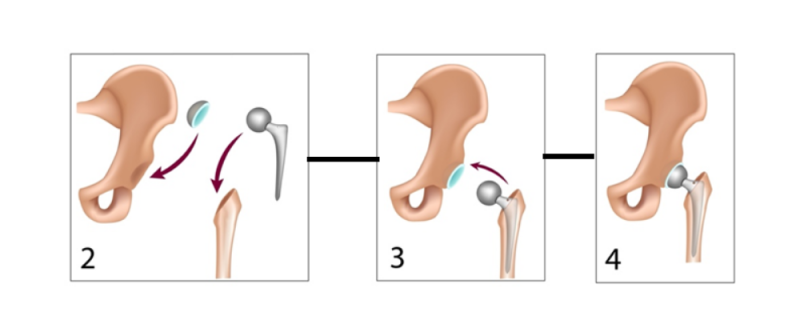
Hip is reduced. Range of movement, leg length and stability are assessed before closing the wound (Fig 4).
Fixation methods – cemented, uncemented or hybrid total hip replacement?
Uncemented, hybrid or cemented fixation techniques are used in total hip replacement. Based on the most suitable fixation technique the total hip replacement can be classified into:
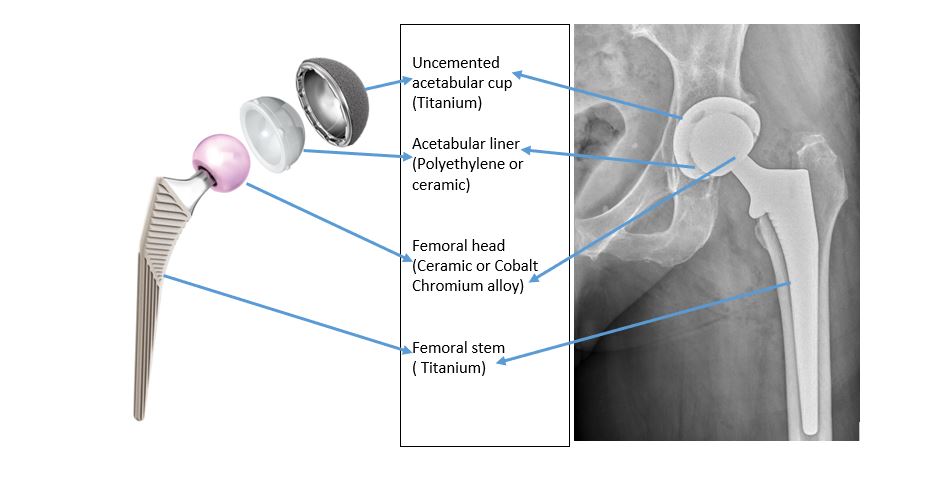
Uncemented total hip replacement – where the acetabular and femur components are fixed without cement. The metal shell or cup (made of Titanium) is seated within the acetabulum (socket) by tight press fit so that the elastic recoil of the bone holds the prostheses temporarily in place until bone grows into the prostheses in a few weeks forming a solid bond. The outer surface of the cup is porous which enables bone ingrowth for fixation. Hydroxy apatite (a calcium compound found in human bone) is also coated onto this surface for better bony ingrowth. A cross-linked high-density polyethylene or ceramic liner is seated within the shell. The femoral stem (made of Titanium) is seated within the prepared femoral canal. Again, the tight press fit is crucial and the porous surface +/- hydroxy apatite coating encourages bone ingrowth. The femoral head component (Ceramic or Cobalt Chromium alloy depending on the type of acetabular cup liner) is attached to the top (called femoral neck or trunnion) of the stem.
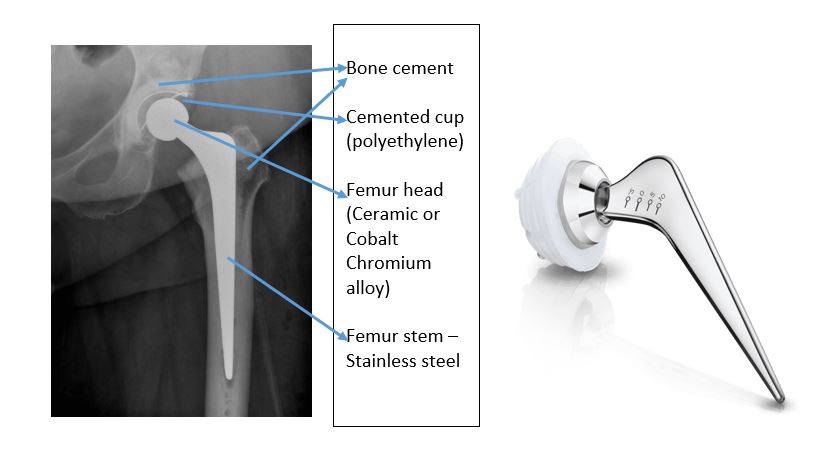
Cemented total hip replacement – where the acetabular (cup) and femur (stem) components are fixed with cement. The polyethylene cup is cemented within the prepared socket. Bone cement (Methyl methacrylate polymer) hardens and fixes the artificial socket (made of cross-linked high-density polyethylene) within the prepared cavity. Similarly, the femoral stem (high quality stainless steel) is cemented within the prepared femoral canal. The femoral head component (Ceramic or Cobalt Chromium alloy) is then attached to the top (called the femoral neck or trunnion) of the stem.
Hybrid total hip replacement – is where the acetabular component is fixed without cement and the femur component is fixed with cement.
Mr Velayudham uses either the uncemented or hybrid technique – whichever gives the best possibility of restoring a patient’s hip anatomy, with low chances of complications and long-term survivorship. He chooses the technique based on the hip anatomy, bone quality and individual patient expectation. He predominantly uses the uncemented technique for both components and, where necessary, uses the hybrid technique. Consensus among hip surgeons in United Kingdom is that the uncemented technique on the acetabular side is better than the cemented technique. There is no real difference between the two techniques on the femoral side. Both cemented and uncemented stems work equally well with equally good long -term results.
What are the hip prostheses made of?
This is a common question asked by patients. Any hip replacement prostheses will have a combination of Titanium, Stainless steel, Cobalt Chromium alloy, Ceramic, cross-linked high-density polyethylene and cement depending on the type of fixation and bearing surface chosen for a patient. These materials cause the least possible biological reaction in the body (bio-inert), having been selected after extensive research over the last six decades and having withstood test of time.
The acetabular component, if it is cemented, is made of cross-linked high-density polyethylene. The inner side of this cemented cup will form the bearing surface. In the uncemented type there are two parts – the shell and the liner. The shell or cup that is fixed within the acetabulum is made of Titanium. The liner that is seated within this uncemented cup forms the bearing surface and is made of either cross-linked high-density polyethylene or ceramic.
The femoral stem component, which is fixed into the femur, is made of Titanium (uncemented) or stainless steel (cemented). The femoral head component (ball) which forms the second bearing surface of the ball and socket construct, is attached to the stem, and articulates with the acetabular liner. This is made of Cobalt Chromium alloy or Ceramic. So, the bearing surface will be a Ceramic head articulating with a Polyethylene or ceramic liner or a Cobalt Chrome alloy head articulating with a Polyethylene liner.
What surgical approach is used for total hip replacement?
Various approaches have been developed to perform total hip replacement and achieve optimal results. Each approach has its advantages and disadvantages. Modern surgical approach techniques have far better recovery and outcomes compared to 20 or 30 years ago. However, there isn’t a significant difference among the current popular minimally invasive surgical approach techniques. The surgeon, based on their training and experience, uses the approach they feel safest.
The approach selected should give the surgeon adequate exposure of the acetabulum and femur to prepare the joint, choose the correct size implants, fix them securely at the correct angles in all three planes, and restore soft tissue tension and leg length. Both surgical approach and accurate placement of the prostheses that are well-fixed are equally important to achieve excellent patient satisfaction and long-term results.
Posterior approach – This is the most common approach used in United Kingdom. The incision is slightly towards the back of the hip. It is more versatile and allows excellent exposure of the acetabulum and femur even in complex cases. Very rare, but possible complications, can be identified and treated safely.
Mr Velayudham uses the Piriformis tendon sparing minimally invasive posterior approach as a default approach. The muscles are pushed aside but not cut. The capsule and ligaments are repaired anatomically to achieve the best possible function. With this approach, fixation technique and prostheses selected for each patient, Mr Velayudham has excellent patient satisfaction and long-term outcomes as confirmed on data collected by National Joint Registry. The data shows outstanding scores for both patient- reported outcomes and long-term function of hip replacement. For some time now, Mr Velayudham has been undertaking successful day case total hip replacement with this approach in selected patients who meet the criteria.
Direct Anterior approach – This incision is directed more towards the front of the hip joint. Access to the hip can be challenging at times. Day case total hip replacement is possible with both direct anterior and minimally invasive posterior approach.
No real evidence exists that either one of these approaches is better than the other. In a small group of patients there may be a slightly better functional score after 6 weeks compared to the posterior approach but there is no discernible functional difference noted between the two groups after 12 weeks.
Clinical results have not shown any significant advantage over the posterior approach. On average one in ten patients may have numbness in part of the thigh due to nerve injury following anterior approach.
Direct Lateral approach – Here the incision is directed more towards the outer aspect of the hip. This approach can compromise the hip muscle (Gluteus medius) function in some patients. Mr Velayudham does not use this approach for this reason.
What are the complications of total hip replacement?
Total hip replacement is a common operation with good to excellent results, but it is not a minor procedure. All surgical procedures have associated risks and complications. There is constant striving to reduce the risks. Precautions are taken by the healthcare team to make every operation as safe as possible, but complications can happen.
Common risks:
Pain: There will be some pain after the hip replacement and regular pain medications will be given. If you are in more pain additional, stronger pain killers will be prescribed. Starting exercises as soon as possible, helps to reduce pain which usually subsides very quickly. In some patients, however, it might last longer but improves at a slower rate. If pain does not respond to routine pain medication, then the hip needs assessing to rule out problems such as fractures, haematoma and infection.
Bleeding: Blood loss is usually minimal. It can be higher in patients who have been on blood thinners prior to surgery. Blood thinners given after surgery to reduce the risk of deep vein thrombosis increase ooze into tissues around the hip. The surgical technique (minimally invasive approach), spinal anaesthesia, stopping the bleeding before closing the wound and Tranexamic acid all help to reduce bleeding.
Occasionally minor ooze from the wound can be seen but it usually stops within a few hours. It is extremely rare to see significant external bleeding from the wound after hip replacement. Bruises might appear spreading down the leg (this varies from person to person) but will get better over the first two to four weeks after the operation.
Major bleeding is uncommon. Major bleeding requiring blood transfusion is very rare. Patients with low haemoglobin prior to surgery have a higher chance of requiring blood transfusion after surgery.
Blood clots (Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)): DVT is a blood clot in a vein. The risk of DVT increases in the legs after lower limb surgery and may present as a red, painful, and swollen leg with or without mild fever. If these symptoms develop then patients should contact the hospital or GP for further assessment and appropriate treatment.
Patients will be given blood-thinning medications for five weeks after surgery to prevent this complication as per NICE guidelines. In a high-risk person for deep vein thrombosis or pulmonary embolism, a higher dose of this medication over a longer period might be considered. Additionally, the use of foot or calf-compression pumps during surgery, and until patients start mobilising, helps to keep blood circulating better and reduces the risk.
There are things that patients themselves can do to reduce the risk. Intermittent walking and exercises while in bed (little and often) are some of the best ways to prevent DVTs from forming. Drinking plenty of water and keeping well-hydrated reduces the risk. Smoking should be avoided. Maintaining a healthy weight at the time of surgery also helps. For more detailed information please follow this link https://orthoinfo.aaos.org/en/diseases–conditions/deep-vein-thrombosis
Urinary retention: Some patients struggle to pass urine after surgery. Occasionally this requires a temporary catheter (tube) to be passed into the bladder. This is common in men with subclinical or clinical prostate-related symptoms. Rarely patients continue to struggle with passing urine and may then need assessment by a urologist.
Constipation: This is not unusual. Laxatives are started on the day of operation to prevent this.
Post-operative delirium: This is common in elderly patients and patients with history of memory loss and Parkinson’s disease. This is also seen in elderly patients with diabetes or kidney disease, and in those patients receiving blood transfusions and on stronger morphine- type pain killers. This usually gets better in two or three days but can last longer.
Acute kidney injury: Abnormal kidney function can happen but is uncommon. The Incidence is higher in patients with pre-existing kidney problems, conditions that can affect kidney functions such as Diabetes, high blood pressure, obesity and in the elderly age group. Blood loss and dehydration after surgery are other risk factors. Hydration is important; patients will receive intravenous fluids until they are eating and drinking well. Blood tests will be done routinely after surgery to detect any blood loss early and treat it if it were to happen.
Less common or Rare:
Infection: Infection can be superficial or deep. Many precautions are taken to avoid infection. Self-hygiene is a very important factor. Advice such as regular showering, change of linens etc., will be discussed in the pre-operative assessment clinic. Preventive measures to avoid any dental, skin and bladder infections should be taken. Patients will be given antibiotics just before the operation. The greatest care is taken to complete the procedure in a clean environment but despite precautions, infection can occur. This needs immediate medical (preferably by the surgeon) attention. Superficial inflammation or infection might fully resolve with a course of antibiotics. Deep infection of the hip replacement is a serious complication and will require further surgery. Strong antibiotics over a longer period might be required. In rare cases, the implants may need to be removed and replaced after the infection is successfully treated. Infection can sometimes lead to sepsis (blood infection).
Soft tissue related pain: Although the hip joint itself has been replaced, the muscles and ligaments around it are the same as before. Just as joints can wear out, the tendons are also prone to wear and can be a source of pain on occasion, for example, gluteus medius tendinopathy. Regular exercises to maintain muscle strength and gentle stretches are key to avoiding or keeping such symptoms under control.
Prosthesis wear and loosening: Statistical evidence on current implants show them lasting 15 to 20 years in 90% of patients. Wear or failure of bearing surfaces and loosening of prostheses fixation are common causes for revision (re-do) total hip replacement. This is a long-term problem. Early loosening is either due to fractures, technical reasons, or infection.
Altered leg length: The leg which has been operated upon may feel longer or, less likely, shorter than the other in the initial few weeks. This sensation usually disappears within a few weeks. Leg length difference is best confirmed directly from your post-operative x-ray. On rare occasions this requires a shoe insert to minimise the difference and in extreme cases further surgery may be required to correct the difference.
Joint dislocation: This used to be a common problem. With current understanding, modern surgical techniques, and pre-operative preparation, the incidence of joint dislocation has reduced. Commonly it is just a one-off episode, and the hip can be reduced under anaesthesia. It is rare nowadays to require surgery to revise the prosthesis, however, patients with certain conditions such as spine stiffness due to arthritis or previous spinal surgery and neuromuscular problems are at high risk of hip dislocation.
Heterotrophic ossification: This is the formation of extra bone around the hip joint after surgery and may lead to pain and/or stiffness. Usually, it is an incidental finding seen on x-rays taken years after surgery and does not bother patients. Rarely this is a reason for persistent pain and very rarely this might result in hip stiffness.
Altered wound healing: The scar may become red, thickened, and painful (keloid scar). Massaging the scar when it has healed can help.
Nerve Damage: Efforts are made to prevent this, however, damage to the nerves around the hip is a risk but again is extremely rare. This may cause temporary or permanent altered sensation and muscle power along the leg. Sciatic nerve injury can affect the foot and ankle. Femoral nerve injury can affect the knee.
Fracture: The thigh bone (Femur), and rarely the pelvis, may break when the prosthesis is inserted. If identified at the time of surgery and fixation is required, this will be carried out. Protected weight-bearing might be necessary if this complication happens. If it is identified on x-rays after surgery, it will be managed by protected weight-bearing for a few weeks with careful monitoring or re-operation where necessary. This is a very rare event, but it is important to be careful in the first few weeks following surgery to avoid trivial injury which can result in this fracture.
Blood vessel damage: Rarely the vessels around the hip may be damaged resulting in the requirement for further surgery by vascular surgeons.
Allergic reaction: Allergic reactions are noted, and all reported medications and equipment are avoided in those patients. For example, using latex-free gloves in patients with latex or kiwi fruit allergy. So, although rare, this can happen without any previous history and can be due to medications given, equipment used and dressing materials. Usually, reactions are very mild and treated promptly. Sometimes treatment will be continued for few days for example, topical applications and antihistamine in patients who develop skin rashes. It is very rare for patients to develop severe allergic reactions.
Pulmonary Embolism (PE): PE is very rare. DVT and PE tend to occur in the first two weeks after surgery and the risks reduce over time. It is very rare occurrence after six weeks post operative.
A DVT can travel through the blood vessels to the lungs causing a pulmonary embolism (PE).
A blood clot that travels to and lodges in the lungs can make breathing very difficult. This is a serious condition which affects breathing and presents as chest or upper back pain, a cough with or without blood in the sputum and difficulty in breathing. If these symptoms develop the patient should go immediately to the hospital Accident & Emergency department. This needs urgent attention and treatment. PE can be fatal.
General Complications: Chest infection, heart complications or stroke can occur after the operation. Patients with pre-existing medical problems such as chronic lung conditions, history of heart problems and history of stroke are at higher risk of such complications. So it is important to get medical problems optimised before any elective surgical procedure.
CoViD-19: In patients who have had a recent attack of CoViD, surgery is delayed by at least seven weeks in order to reduce the risk of chest infection and other chest complications.
Death: Loss of life can occur from any of the above complications. The risk is increased by underlying medical conditions and advanced age.
